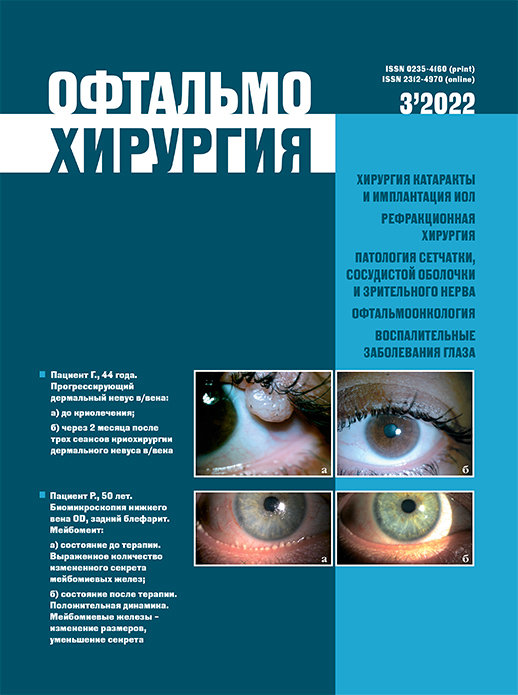
Диагностика синдрома лимбальной недостаточности
Ключевые слова:
синдром лимбальной недостаточности, импрессионная цитология, лазерная сканирующая конфокальная микроскопия, бокаловидные клетки, цитокератины, сквозная кератопластика, цитокиныАннотация
Актуальность. Синдром лимбальной недостаточности (СЛН) является патологией, приводящей к снижению зрения, развитию неоваскуляризации роговицы, появлению персистирующих эрозий и негативному воздействию на качество жизни пациента. Известно, что эффективность трансплантации роговицы при этом невысока и требует неоднократных повторных вмешательств. Одной из важных проблем, является отсутствие четкого алгоритма диагностики и стандартизированного набора методов исследований для данного заболевания. Цель. Подробное изложение основных методов диагностики СЛН.
Материал и методы. Произведен системный анализ научных публикаций отечественных и зарубежных авторов на ресурсах PubMed, Medline, eLibrary, а также диссертационных работ и учебников c 1992 до 2021 г., посвященных существующим на настоящий момент методам диагностики СЛН.
Результаты. Основными прижизненными методами диагностики СЛН помимо биомикроскопии являются: окрашивание глазной поверхности, импрессионная цитология с выявлением специфических цитокератинов, конфокальная микроскопия, оптическая когерентная томография (ОКТ) переднего отрезка и ОКТ-ангиография.
Заключение. У пациентов с конъюнктивализацией и васкуляризацией роговицы следует проявлять настороженность и проводить дополнительную диагностику на предмет наличия СЛН. Диагностика данного заболевания должна быть комплексной и, помимо сбора анамнеза и биомикроскопии с обязательной прижизненной окраской (флюоресцеин), включать инструментальные исследования, основанные на детальной визуализации переднего отрезка глаза с высоким разрешением (ОКТ, конфокальная микроскопия), а также лабораторной диагностике (цитология, иммуноцитохимия).
Библиографические ссылки
1. Deng SX, Borderie V, Chan CC, Dana R, Figueiredo FC, Gomes JAP, Pellegrini G, Shimmura S, Kruse FE; and The International Limbal Stem Cell Deficiency Working Group. Global consensus on definition, classification, diagnosis, and staging of limbal stem cell deficiency. Cornea. 2019;38(3): 364 375. doi: 10.1097/ICO.0000000000001820
2. Тонаева Х.Д., Онищенко Н.А., Борзенок С.А. Лимбальная трансплантация как способ индукции локальной иммунной толерантности при кератопластике высокого риска. Вестник трансплантологии и искусственных органов. 2011;8: 95–102. doi: 10.15825/1995-1191-2011-2-95-102. [Tonaeva KD, Onishchenko NA, Borzenok SA. Limbal transplantation as a method of local immune tolerance induction in high risk keratoplasty. Russian Journal of Transplantology and Artificial Organs. 2011;13(2): 95–102. (In Russ.)]
3. Puangsricharern V, Tseng SC. Cytologlogic evidence of corneal diseases with limbal stem cell deficiency. Ophthalmology. 1995;102(10): 1476–1485. doi: 10.1016/ s0161-6420(95)30842-1
4. Sacchetti M, Lambiase A, Cortes M, Sgrulletta, R, Bonini S, Merlo D, Bonini S. Clinical and cytological findings in limbal stem cell deficiency. Graefes Arch Clin Exp Ophthalmol. 2005;243(9): 870–876. doi: 10.1007/s00417-005-1159-0
5. Deng S, Sejpal K, Bakhtiari P. Presentation, diagnosis and management of limbal stem cell deficiency. Middle East Afr J Ophthalmol. 2013;20(1): 5–10. doi: 10.4103/0974-9233.106381
6. Dua HS, Saini JS, Azuara-Blanco A, Gupta P. Limbal stem cell deficiency: concept, aetiology, clinical presentation, diagnosis and management. Indian J Ophthalmol. 2000;48(2): 83–92.
7. Черныш В.Ф., Бойко В.Ф. Ожоги глаз – состояние проблемы и новые подходы. М.: ГЭОТАР-Медиа; 2008. [Chernikh VF, Boyko VF. Eye burns – the state of the problem and new approaches. M.: GEOTAR-Media; 2008. (In Russ.)]
8. Holland EJ, Schwartz GS. The evolution of epithelial transplantation for severe ocular surface disease and a proposed classification system. Cornea. 1996;15(6): 549–556.
9. Zuazo F, Lopez-Ponce D, Salinas-Toro D, Valenzuela F, Sans-Puroja J, Srur M, López-Solís RO, Traipe-Castro L. Conjunctival impression cytology in patients with normal and impaired OSDI scores. Arch Soc Esp Oftalmol. 2014;89(10): 391–396. doi: 10.1016/j.oftal.2014.04.013
10. Чирский В.С., Чурашов С.В., Злобин И.А., Рудько А.С., Черныш В.Ф., Курносов В.Е. Роль импрессионной цитологии в оценке фенотипа эпителия роговицы при решении вопроса о показаниях к операции оптической кератопластики. Вестник Российской Военно-Медицинской Академии. 2016;1(53): 89–93. [Zlobin IA, Chernysh VF, Churashov SV, Chirsky VS, Rudko AS, Kurnosov VE. Role of impression cytology in cornea epithelium phenotype assessment at solution of question of indications to operation of optical keratoplasty. Bulletin of Russian Military Medical Academy. 2016;1(53): 89–93. (In Russ.)]
11. Krenzer KL, Freddo TF. Cytokeratin expression in normal human bulbar conjunctiva obtained by impression cytology. Invest Ophthalmol Vis Sci. 1997;38(1): 142–152.
12. Barbaro V, Ferrari S, Fasolo A, Pedrotti E, Marchini G, Sbabo A, Nettis N, Ponzin D, Di Iorio E. Evaluation of ocular surface disorders: a new diagnostic tool based on impression cytology and confocal laser scanning microscopy. Br J Ophthalmol. 2010;94(7): 926–932. doi: 10.1136/bjo.2009.164152
13. Le Q, Xu J, Deng SX. The diagnosis of limbal stem cell deficiency. The Ocular Surface. 2018;16(1): 58–69. doi:10.1016/j.jtos.2017.11.002
14. Dua HS, Joseph A, Shanmuganathan VA, Jones RE. Stem cell differentiation and the effects of deficiency. Eye (Lond). 2003;17(8): 877–885. doi: 10.1038/sj.eye.6700573
15. Rossen J, Amram A, Milani B, Park D, Harthan J, Joslin C, McMahon T, Djalilian A. Contact lens-induced limbal stem cell deficiency. Ocul Surf. 2016;14(4): 419–434. doi: 10.1016/j.jtos.2016.06.003
16. Deng SX, Sejpal KD, Tang Q, Aldave AJ, Lee OL, Yu F. Characterization of limbal stem cell deficiency by in vivo laser scanning confocal microscopy: a microstructural approach. Arch Ophthalmol. 2012;130(4): 440–445. doi: 10.1001/ archophthalmol.2011.378
17. Efron Contact Lens Complications 4th Ed. Elsevier; 2019: 366–2010.
18. Lakkis C, Brennan NA. Bulbar conjunctival fluorescein staining in hydrogel contact lens wearers. CLAO J. 1996;22(3): 189–194.
19. Norn MS. Fluorescein vital staining of the cornea and conjunctiva. Studied by triple staining with fluorescein, rose Bengal, and alcian blue. Acta Ophthalmol (Copenh). 1964;42: 1038–1045.
20. Dua HS. The conjunctiva in corneal epithelial wound healing. Br J Ophthalmol. 1998;82(12): 1407–1411. doi: 10.1136/bjo.82.12.1407
21. Chan CC, Holland EJ. Severe limbal stem cell deficiency from contact lens wear: patient clinical features. Am J Ophthalmol. 2013;155(3): 544-549.e2. doi: 10.1016/j. ajo.2012.09.013.
22. Guillon M, Maissa C. Bulbar conjunctival staining in contact lens wearers and non-lens wearers and its association with symptomatology. Cont Lens Anterior Eye. 2005;28(2): 67–73. doi: 10.1016/j.clae.2005.02.002
23. Fatimа A, Iftekhar G, Sangwan VS and Vemuganti GK. Ocular surface changes in limbal stem cell deficiency caused by chemical injury: a histologic study of excised pannus from recipients of cultured corneal epithelium. Eye (Lond). 2008;22:(9): 1161–1167. doi:10.1038/sj.eye.6702895
24. Sati A, Basu S, Sangwan VS, Vemuganti GK. Correlation between the histological features of corneal surface pannus following ocular surface burns and the final outcome of cultivated limbal epithelial transplantation. Br J Ophthalmol. 2015;99(4): 477–481. doi:10.1136/bjophthalmol-2014-305568
25. Волкович Т.К., Самсонова И.В., Имшенецкая Т.А., Залуцкий И.В. Импрессионная цитология: диагностические возможности в офтальмологии. Российская детская офтальмология. [Volkovich TK, Samsonova IV, Imshenetskaya TA, Zalutsky IV. Impression cytology: diagnostic possibilities in ophthalmology. Russian Pediatric Ophthalmology. 2016;1: 46–52. (In Russ.)]
26. Zuazo F, López-Ponce D, Salinas-Toro D, Valenzuela F, Sans-Puroja J, Srur M, López-Solís RO, Traipe-Castro L. Conjunctival impression cytology in patients with normal and impaired OSDI scores. Arch Soc Esp Oftalmol. 2014;89(10): 391–396. doi: 10.1016/j.oftal.2014.04.013
27. Egbert PR, Lauber S, Maurice DM. A simple conjunctival biopsy. Am J Ophthalmol. 1977;84(6): 789–801. doi: 10.1016/0002-9394(77)90499-8
28. Singh R, Joseph A, Umapathy T, Tint NL, Dua HS. Impression cytology of the ocular surface. Br J Ophthalmol. 2005;89(12): 1655–1659. doi: 10.1136/ bjo.2005.073916
29. Tseng SCG. Staging of conjunctival squamous metaplasia by impression cytology. Ophthalmology. 1985;92(6): 728–733. doi: 10.1016/s0161 6420(85)33967-2
30. Maskin SL, Bode DD. Electron microscopy of impression-acquired conjunctival epithelial cells. Ophthalmology. 1986;93(12): 1518–23. doi: 10.1016/s0161-6420(86)33538-3
31. Prabhasawat P, Tseng SCG. Impression cytology study of epithelial phenotype of ocular surface reconstructed by preserved human amniotic membrane. Arch Ophthalmol. 1997;115(11): 1360–1367. doi: 10.1001/archopht.1997.01100160530001
32. Shimazaki J, Yang H, Tsubota K. Amniotic membrane transplantation for ocular surface reconstruction in patients with chemical and thermal burns. Ophthalmology. 1997;104(12): 2068–2076. doi: 10.1016/s0161-6420(97)30057-8
33. Dua HS, King AJ, Joseph A. A new classification of ocular surface burns. Br J Ophthalmol. 2001;85(11): 1379–1383. doi: 10.1136/bjo.85.11.1379
34. Jirsova K, Dudakova L, Kalasova S, et al. The OV-TL 12/30 clone of anticytokeratin 7 antibody as a new marker of corneal conjunctivalization in patients with limbal stem cell deficiency. Invest Ophthalmol Vis Sci. 2011;52(8): 5892–5898. doi: 10.1167/iovs.10-6748
35. Ramirez-Miranda A, Nakatsu MN, Zarei-Ghanavati S, et al. Keratin 13 is a more specific marker of conjunctival epithelium than keratin 19. Mol Vision. 2011;17: 1652–1661.
36. Wei ZG, Wu RL, Lavker RM, et al. In vitro growth and differentiation of rabbit bulbar, fornix, and palpebral conjunctival epithelia. Implications on conjunctival epithelial transdifferentiation and stem cells. Invest Ophthalmol Vis Sci. 1993;34(5):1814–1828.
37. Muriel P, Helene J, Virginie J, Celine A, Carole B, Odile D. Keratin 13 immunostaining in corneal impression cytology for the diagnosis of limbal stem cell deficiency. Invest Ophthalmol Vis Sci. 2011;52(13): 9411–9415. doi: 10.1167/iovs.10- 7049
38. Poli M, Burillon C, Auxenfans C, Rovere M, Damour O. Immunocytochemical diagnosis of limbal stem cell deficiency: comparative analysis of current corneal and conjunctival biomarkers. Cornea. 2015;34(7): 817–823. doi: 10.1097/ ICO.0000000000000457
39. Chuephanich P, Supiyaphun C, Aravena C, Bozkurt T, Yu F, Deng SX. Characterization of the corneal subbasal nerve plexus in limbal stem deficiency. Cornea. 2017;36(3): 347–352. doi: 10.1097/ICO.0000000000001092
40. Colorado LH, Alzahrani Y, Pritchard N, Efron N. Assessment of conjunctival goblet cell density using laser scanning confocal microscopy versus impression cytology. Cont Lens Anterior Eye. 2016;39(3): 221–226. doi: 10.1016/j.clae.2016.01.006
41. Garcia I, Etxebarria J, Boto-de-Los-Bueis A, Díaz-Valle D, Rivas L, Martínez-Soroa I, Saenz N, López C, Del-Hierro-Zarzuelo A, Méndez R, Soria J, González N, Suárez T, Acera A. Comparative study of limbal stem cell deficiency diagnosis methods: detection of MUC5AC mRNA and goblet cells in corneal epithelium. Ophthalmology. 2012;119(5): 923–929. doi: 10.1016/j.ophtha.2011.10.031
42. Le Q, Chauhan T, Deng, SX. Diagnostic criteria for limbal stem cell deficiency prior to surgical intervention. A systematic literature review and analysis. Surv Ophthalmol. 2020;65(1): 32–40. doi: 10.1016/j.survophthal.2019.06.008
43. Vadrevu VL, Fullard RJ. Enhancements to the conjunctival impression cytology technique and examples of applications in a clinico-biochemical study of dry eye. CLAO J. 1994;20(1): 59–63.
44. Chan E, Le Q, Codriansky A, Hong J, Xu J, Deng SX. Existence of normal limbal epithelium in eyes with clinical signs of total limbal stem cell deficiency. Cornea. 2016;35(11): 1483–1487. doi: 10.1097/ICO.0000000000000914
45. Nubile M, Lanzini M, Miri A, Pocobelli A, Calienno R, Curcio C, Mastropasqua R, Dua HS, Mastropasqua L. In vivo confocal microscopy in diagnosis of limbal stem cell deficiency. Am J Ophthalmol. 2013;155(2): 220–232. doi: 10.1016/j.ajo.2012.08.017
46. Wang Y, Le Q, Zhao F, Hong J, Xu J, Zheng T, Sun X. Application of in vivo laser scanning confocal microscopy for evaluation of ocular surface diseases: lessons learned from pterygium, meibomian gland disease, and chemical burns. Cornea. 2011;30(suppl 1): 25–S28. doi: 10.1097/ICO.0b013e318227fcd9
47. Cruzat A, Pavan-Langston D, Hamrah P. In vivo confocal microscopy of corneal nerves: analysis and clinical correlation. Semin Ophthalmol. 2010;25(5–6): 171–177. doi: 10.3109/08820538.2010.518133
48. Lum E, Golebiowski B, Swarbrick HA. Mapping the corneal sub-basal nerve plexus in orthokeratology lens wear using in vivo laser scanning confocal microscopy. Invest Ophthalmol Vis Sci. 2012;53(4): 1803–1809. doi: 10.1167/iovs.11-8706
49. Nubile M, Lanzini M, Miri A, Pocobelli A, Calienno R, Curcio C, Mastropasqua R, Dua HS, Mastropasqua L. In vivo confocal microscopy in diagnosis of limbal stem cell deficiency. Am J Ophthalmol. 2013;155(2): 220–32. doi: 10.1016/j.ajo.2012.08.017
50. Vera LS, Gueudry J, Delcampe A, Roujeau, JC, Brasseur G, Muraine M. In vivo confocal microscopic evaluation of corneal changes in chronic Stevens Johnson syndrome and toxic epidermal necrolysis. Cornea. 2009;28(4): 401–7. doi: 10.1097/ ICO.0b013e31818cd299
51. Zhivov A, Winter K, Hovakimyan M, Peschel S, Harder V, Schober HC, Kundt G, Baltrusch S, Guthoff RF, Stachs O. Imaging and quantification of subbasal nerve plexus in healthy volunteers and diabetic patients with or without retinopathy. PLoS One. 2013;8(1): e52157. doi: 10.1371/journal.pone.0052157
52. Lagali N. Laser-scanning in vivo confocal microscopy of the cornea: imaging and analysis methods for preclinical and clinical applications. In: Lagali N (ed.) Confocal laser microscopy. Principles and applications in medicine, biology, and the food sciences. London, UK: IntechOpen Limited; 2013: 51 80.
53. Chan EH, Chen L, Rao JY, Fei Y, Deng, SX. Limbal basal cell density decreases in limbal stem cell deficiency. Am J Ophthalmol. 2015;160(4):678–84.e4. doi: 10.1016/j. ajo.2015.06.026
54. Chan EH, Chen L, Yu F, Deng SX. Epithelial thinning in limbal stem cell deficiency. Am J Ophthalmol. 2015;160(4): 669–77.e4. doi: 10.1016/j.ajo.2015.06.029
55. Patel DV, Sherwin T, Mcghee CN. Laser scanning in vivo confocal microscopy of the normal human corneoscleral limbus. Invest Ophthalmol Vis Sci. 2006; 47(7): 2823–2827. doi: 10.1167/iovs.05-1492
56. Miri A, Al-aqaba M, Otri AM, Fares U, Said DG, Faraj LA, Dua HS. In vivo confocal microscopic features of normal limbus. Br J Ophthalmol. 2012;96(4): 530–536. doi: 10.1136/bjophthalmol-2011-300550
57. Паштаев Н.П., Куликова И.Л., Шленская О.В., Волкова Л.Н. Конфокальная микроскопия роговицы в кераторефракционной хирургии. Обзор литературы. Вестник ТГУ. 2015:20(3): 662–666. [Pashtaev NP, Kulikova IL, Shlenskaya OV, Volkova LN. Confocal microscopy of the cornea in keratorefrctive surgery. Literature review. 2015;20(3): 662–666. (In Russ.)]
58. Bizheva K, Hutchings N, Sorbara L, Moayed AA, Simpson T. In vivo volumetric imaging of the human corneo-scleral limbus with spectral domain OCT. Biomed OptExpress. 2011;2(7): 1794–1702. doi: 10.1364/BOE.2.001794
59. Romano A, Espana EM, Djalilian AR, Yoo SH. En face optical coherence tomography imaging of corneal limbal stem cell niche. In: Lumbroso B, Huang D, Romano A, Rispoli M, Coscas G (ed.). Clinical en face OCT atlas. New Delhi, India: Jaypee Brothers Medical Publishers Ltd; 2013: 77–79.
60. Haagdorens M, Behaegel J, Rozema J, Van Gerwen V, Michiels S, Ní Dhubhghaill S, Tassignon MJ, Zakaria N. A method for quantifying limbal stem cell niches using OCT imaging. Br J Ophthalmol. 2017;101(9): 1250–1255. doi: 10.1136/ bjophthalmol-2016-309549
61. Bizheva K, Tan B, MacLellan B, Hosseinaee Z, Mason E, Hileeto D, Sorbara L. Invivo imaging of the palisades of Vogt and the limbal crypts with sub micrometer axial resolution optical coherence tomography. Biomed Opt Express. 2017;8(9): 4141–4151. doi: 10.1364/BOE.8.004141
62. Le Q, Yang Y, Deng SX, Xu J. Correlation between the existence of the palisades of Vogt and limbal epithelial thickness in limbal stem cell deficiency. Clin Exp Ophthalmol. 2017;45(3): 224–231. doi: 10.1111/ceo.12832
63. Zakaria N, Ni Dhubhghaill S, Taal M, Berneman Z, Koppen C, Tassignon MJ. Optical coherence tomography in cultivated limbal epithelial stem cell transplantation surgery. Asia Pac J Ophthalmol (Phila). 2015;4(6): 339–345. doi: 10.1097/ APO.0000000000000163
64. Banayan N, Georgeon C, Grieve K, Borderie, VM. Spectral domain optical coherence tomography in limbal stem cell deficiency: A case control study. Am J Ophthalmol. 2018;190: 179–190. doi: 10.1016/j.ajo.2018.03.034
65. Воскресенская А.А., Поздеева Н.А., Шипунов А.А., Гаглоев Б.В. Диагностические возможности оптической когерентной томографии в визуализации лимбальных палисад Фогта. Современные технологии в офтальмологии. 2017;3: 103–106. [Voskresenskaya AA, Pozdeeva NA, Shipunov AA, Gagloev BV. Diagnostic capabilities of optical coherence tomography in visualization of limbal palisades of Vogt. Modern technology in ophthalmology. 2017;3: 103–106. (In Russ.)]
66. Liang Q, Le Q, Cordova DW, Tseng CH, Deng SX. Corneal epithelial thickness measured using anterior segment optical coherence tomography as a diagnostic parameter for limbal stem cell deficiency. Am J Ophthalmol. 2020;216: 132–139. doi: 10.1016/j.ajo.2020.04.006
67. Jia Y, Bailey ST, Hwang TS, McClintic SM, Gao SS, Pennesi ME, Flaxel CJ, Lauer AK, Wilson DJ, Hornegger J, Fujimoto JG, Huang D. Quantitative optical coherence tomography angiography of vascular abnormalities in the living humaneye. Proc Natl Acad Sci USA. 2015;112(18): 2395–2402. doi: 10.1073/pnas.1500185112
68. Ang M, Sim DA, Keane PA, Sng, CC, Egan, CA, Tufail A, Wilkins MR. Optical coherence tomography angiography for anterior segment vasculature imaging. Ophthalmology. 2015;122(9): 1740–1747. doi: 10.1016/j.ophtha.2015.05.017
69. Oie Y, Nishida K. Evaluation of corneal neovascularization using optical coherence tomography angiography in patients with limbal stem cell deficiency. Cornea. 2017;36(suppl 1): 72–75. doi: 10.1097/ICO.0000000000001382
70. Nanji A, Redd T, Chamberlain W, Schallhorn JM, Chen S, Ploner S, Maier A, Fujimoto JG, Jia Y, Huang D, Li Y. Application of corneal optical coherence tomography angiography for assessment of vessel depth in corneal neovascularization. Cornea. 2020;39(5): 598–604. doi: 10.1097/ICO.0000000000002232
71. Binotti WW, Nosé RM, Koseoglu ND, Dieckmann GM, Kenyon K, Hamrah P. The utility of anterior segment optical coherence tomography angiography for the assessment of limbal stem cell deficiency. Ocul Surf. 2021;19: 94–103. doi: 10.1016/j. jtos.2020.04.007
72. Varma S, Shanbhag SS, Donthineni PR, Mishra DK, Singh V, Basu S. Highresolution optical coherence tomography angiography characteristics of limbal stem cell deficiency. Diagnostics. 2021;11(6): 1130. doi: 10.3390/diagnostics11061130
73. Maguire MG, Stark WJ, Gottsch JD, Stulting RD, Sugar A, Fink NE Schwartz A. Risk factors for corneal graft failure and rejection in the collaborative corneal transplantation studies. Collaborative Corneal Transplantation Studies Research Gro up. Ophthalmology. 1994;101(9): 1536–1547. doi: 10.1016/s0161-6420(94)31138-9
74. Sangwan VS, Ramamurthy B, Shah U, Garg P, Sridhar MS, Rao GN. Outcome of corneal transplant rejection: a 10-year study. Clin Experiment Ophthalmol. 2005;33(6): 623–627. doi: 10.1111/j.1442-9071.2005.01107.x
75. Holland EJ, Djalilian AR, Schwartz GS. Management of aniridic keratopathy with keratolimbal allograft: a limbal stem cell transplantation technique. Ophthalmology. 2003;110(1): 125–130. doi: 10.1016/s0161-6420(02)01451-3
76. Ramaesh K, Ramaesh T, Dutton GN, Dhillon B. Evolving concepts on the pathogenic mechanisms of aniridia related keratopathy. Int J Biochem Cell Biol. 2005;37(3): 547–557. doi: 10.1016/j.biocel.2004.09.002
77. Каспаров А.А. Офтальмогерпес. М., Издательство «Медицина»; 1994: 224. [Kasparov AA. Ophthalmogerpes. M.: Izdatel’stvo «Medicina»; 1994: 224. (In Russ.)]
78. Комах Ю.А., Мороз З.И., Борзенок С.А. Современное состояние проблемы повторной пересадки роговицы (обзор литературы). Офтальмохирургия.1997;(1): 19–27. [Komakh YA, Moroz ZI, Borzenok SA. The current state of the problem of repeated corneal transplantation (literature review). Fyodorov Journal of Ophthalmic Surgery. 1997;(1): 19–27. (In Russ.)]
79. Малюгин Б.Э., Герасимов М.Ю., Борзенок С.А., Головин А.В. Клеточная хирургия при дисфункции стволовых клеток лимба. Офтальмохирургия. 2019;1: 77–86. https://doi.org/10.25276/0235-4160-2019-1-77-86 [Malyugin BE, Gerasimov MYu, Borzenok SA, Golovin AV. Cellular surgery for limb stem cell dysfunction. Fyodorov Journal of Ophthalmic Surgery. 2019;1: 77–86. https://doi.org/10.25276/0235-4160-2019-1-77- 86 (In Russ.)]
80. Пирогов Ю.И., Дронов М.М., Першин К.Б., Пашинова Я.Ф., Азербаев Т.Э., Першин Б.Б. Состояние иммунитета при заболеваниях, травмах и трансплантации роговицы. Офтальмохирургия и терапия. 2002;2: 29–47. [Pirogov JU, Drovon MM, Perchin KB, Pachinova NF, Aserbaev TE, Perchin BB. Immune status during diseases, traumas and cornea transplantations. Ophthalmochirurgia and therapy. 2002;2: 29–47. (In Russ.)]
81. Biswas S, Suresh P, Bonshek RE, Corbitt G, Tullo AB, Ridgway AE. Graft failure in human donor corneas due to transmission of herpes simplex virus. Br J Ophthalmol. 2000;84(7): 701–705. doi: 10.1136/bjo.84.7.701
82. Guilbert E, Laroche L, Borderie V. Rejection of corneal allografts. Fr Ophthalmol. 2011;34(5): 331–348. doi: 10.1016/j.jfo.2011.02.001
83 Khodadoust AA, AbKizadeh A. The rate of corneal rejection after previous rejection reaction. In: Silverstein AM, O’Connor GR (eds.). Immunology and immunopathology of the eye. New York, Masson; 1979: 271–283.
84. Zierhut M, Pleyer U, Thiel HJ. Immunology of corneal transplantation. Amsterdam, Aeolus Press; 1994: 233–238.
85. Rumelt S, Bersudsky V, Blum-Hareuveni T, Rehany U. Systemic cyclosporine A in high failure risk, repeated corneal transplantation. Br J Ophthalmol. 2002;86(9): 988–992. doi: 10.1136/bjo.86.9.988
86. Polisetty N, Fatima A, Madhira SL, Sangwan VS, Vemuganti GK. Mesenchymal cells from limbal stroma of human eye. Mol Vis. 2008;4(14): 431–442.
87. Panda A, Vanathi M, Kumar A, Dash, Y, Priya S. Corneal graft rejection. Surv Ophthalmol. 2007;52(4): 375–396. doi: 10.1016/j.survophthal.2007.04.008
88. Kaminska A, Szaflik J, Minkiewicz-Timler G, Sybilska M, Pawluczyk-Dyjecinska M, Cieslik K. Retrospective evaluation of risk factors for graft rejection in patients after corneal transplantation performed at the Eye Clinic in the years 2001–2003. Klin Oczna. 2005;107(4–6): 209–211.
89. Hill JC. The relative importance of risk factors used to define high-risk keratoplasty. Ger J Ophthalmol. 1996;5(1): 36–41.
90. De Freitas AM, Melo BC, Mendonca CN, Machado RP, Rocha FJ. Causes and risk factors for graft failure in surgeries performed by physicians in fellowship training. Cornea. 2006;25(3): 251–256. doi: 10.1097/01.ico.0000222480.45371.31
91. Maguire MG, Stark WJ, Gottsch JD, Stulting RD, Sugar A, Fink NE, Schwartz A. Risk factors for corneal graft failure and rejection in the collaborative corneal transplantation studies. Collaborative сorneal transplantation studies research group. Ophthalmology. 1994;101(9): 1536–1547. doi: 10.1016/s0161-6420(94)31138-9
92. Bachmann B, Taylor RS, Cursiefen C. Corneal neovascularization as a risk factor for graft failure and rejection after keratoplasty: an evidence-based meta-analysis. Ophthalmology. 2010;117(7): 1300–1305.e7. doi: 10.1016/j. ophtha.2010.01.039
93. Иммунология глазной патологии. Под ред. Пучковской Н.А., Шульгиной Н.С., Минеева Н.Г., Игнатова Р.К. Издательство «Медицина»; 1983. [Immunology of ocular pathology. Puchkovskaya NA, Shulgina NS, Mineev NG, Ignatov RK (eds.). M.: Izdatel’stvo «Medicina»; 1983. (In Russ.)]
94. Волков В.В., Хавинсон В.Х., Пасхина М.Н., Пирогов Ю.И. Иммунологическая диагностика и прогнозирование приживления кератотрансплантатов. Вестник офтальмологии. 1986;5: 27–31. [Volkov VV, Havinson VH, Pashina MN, Pirogov YI. Immunological diagnostics and prediction of keratograft engraftment. The Russian Annals of Ophthalmology. 1986;5: 27–31. (In Russ.)]
95. Roy R, Boisjoly HM, Wagner E, Langlois A, Bernard PM, Bazin R, Laughrea PA, Dubé I. Pretransplant and posttransplant antibodies in human corneal transplantation. Transplantation. 1992;54(3): 463–467. doi: 10.1097/00007890-199209000-00015
96. Malyugin BE, Gerasimov MY, Borzenok SA. Glueless simple limbal epithelial transplantation (G-SLET). The report of the first two cases. CORNEA. 2020;39: 1588-1591. https://doi.org/10.1097/ICO.0000000000002467
97. Слепова О.С. Практическое значение исследования цитокинов при заболеваниях глаз. VII Всероссийский съезд офтальмологов России. Материалы съезда. М.;2000: 159–160. [Slepova OS. Practical significance of cytokine research in eye diseases. VII All-Russian Congress of Ophthalmologists of Russia. Materials of the congress. M.; 2000: 159–160. (In Russ.)]
98. Kim KH, Park SW, Kim MK, et al. Effect of age and early intervention with a systemic steroid, intravenous immunoglobulin or amniotic membrane transplantation on the ocular outcomes of patients with Stevens – Johnson syndrome. Korean J Ophthalmol. 2013;27(5): 331–340. doi: 10.3341/kjo.2013.27.5.331
99. Ohji M, Ohmi G, Kiritoshi A, Kinoshita S. Goblet cell density in thermal and chemical injuries. Arch Ophthalmol. 1987;105(12): 1686–1688. doi: 10.1001/ archopht.1987.01060120084031
100. Chen Z, de Paiva CS, Luo L, Kretzer FL, Pflugfelder SC, Li D Q. Characterization of putative stem cell phenotype in human limbal epithelia. Stem Cells. 2004;22(3): 355–366. doi: 10.1634/stemcells.22-3-355
101. Kasper M, Moll R, Stosiek P, Karsten U. Patterns of cytokeratin and vimentin expression in the human eye. Histochemistry. 1988;89(4): 369–377. doi: 10.1007/BF00500639
102. Yoshida S, Shimmura S, Kawakita T, Miyashita H, Den S, Shimazaki J, Tsubota K. Cytokeratin 15 can be used to identify the limbal phenotype in normal and diseased ocular surfaces. Invest Ophthalmol Vis Sci. 2006;47(11): 4780–4786. doi: 10.1167/ iovs.06-0574
Опубликован
Лицензия

Это произведение доступно по лицензии Creative Commons «Attribution-NonCommercial» («Атрибуция — Некоммерческое использование») 4.0 Всемирная.